From The Blog
Men's Fertility and Infertility
Starting a family is an exciting milestone that many couples dream about. Yet, the journey to parenthood isn’t always straightforward, especially when fertility challenges arise. Like many couples, you may find yourself facing unexpected hurdles while trying to conceive.
We understand that fertility issues can be overwhelming, and they’re often unfairly attributed to women, which is why proper knowledge about male fertility is crucial and should be openly discussed. Male factors actually contribute to half of all infertility cases, with men being solely responsible in ⅓ or 30% of cases and partially responsible in another 30-40% of cases. This is why both partners need thorough evaluation when conception becomes challenging.
For couples trying to conceive, medical professionals recommend seeking a fertility evaluation if pregnancy hasn’t occurred after 12 months of regular, unprotected intercourse, assuming neither partner is using contraception.
Let us guide you through understanding male fertility and infertility. You’ll discover how doctors diagnose infertility (typically after one year of unprotected intercourse without conception), what success rates look like for different age groups, and why timing matters – as healthy couples under 30 have a 20-37% chance of conceiving within just three months. This knowledge will empower you to make informed decisions about your reproductive health journey.
Let’s begin.
Understanding Male Reproductive System
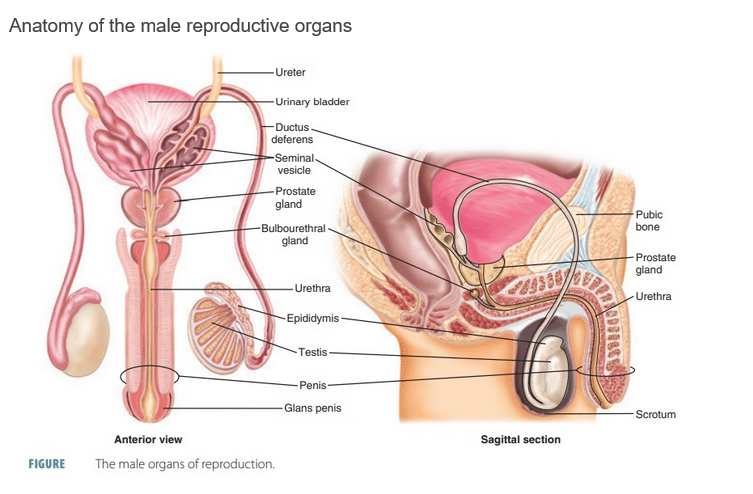
The male reproductive system is a sophisticated network of organs that work together to create and deliver healthy sperm for reproduction. This system relies on both physical organs and hormonal signals from the brain to function properly.
The male reproductive system consists of several organs:
- Ureter: Tube that carries urine from kidneys to bladder
- Urinary bladder: Organ that stores urine before excretion
- Ductus deferens: Also called vas deferens, tubes that transport sperm
- Seminal vesicle: Gland that produces components of seminal fluid
- Prostate gland: Produces fluid that helps nourish and transport sperm
- Bulbourethral gland: Produces clear fluid that lubricates the urethra
- Urethra: Tube that carries both urine and semen out of the body
- Epididymis: Coiled tube where sperm mature and are stored
- Testis: Produces sperm and male hormones
- Penis: Male reproductive and urinary organ
- Glans penis: Sensitive tip of the penis
- Pubic bone: Part of the pelvis that protects reproductive organs
- Scrotum: External sac containing the testes
Physiology of sperm production (spermatogenesis)
Sperm production, known as spermatogenesis, takes place within the testes over approximately 74 days. This process begins with special stem cells multiplying, followed by a precise cell division called meiosis that creates cells with half the normal genetic material. These cells then transform from round shapes into the streamlined sperm cells needed for fertilization.
Hormonal regulation of male fertility
The entire system operates under careful hormonal control. The hypothalamus in the brain releases gonadotropin-releasing hormone (GnRH), which signals the pituitary gland to produce follicle-stimulating hormone (FSH) and luteinizing hormone (LH).
These hormones then trigger the testes to produce testosterone and maintain sperm production, creating a synchronized chain of signals that keeps the reproductive system running smoothly.
Factors Affecting Male Fertility
Infertility has become prevalent, with studies showing that 1 in 6 to 1 in 10 sexually active couples face challenges conceiving. The past ten years have seen a significant rise in the number of couples seeking professional help for fertility-related concerns.
Factors Affecting Male Fertility
Infertility has become prevalent, with studies showing that 1 in 6 to 1 in 10 sexually active couples face challenges conceiving. The past ten years have seen a significant rise in the number of couples seeking professional help for fertility-related concerns.
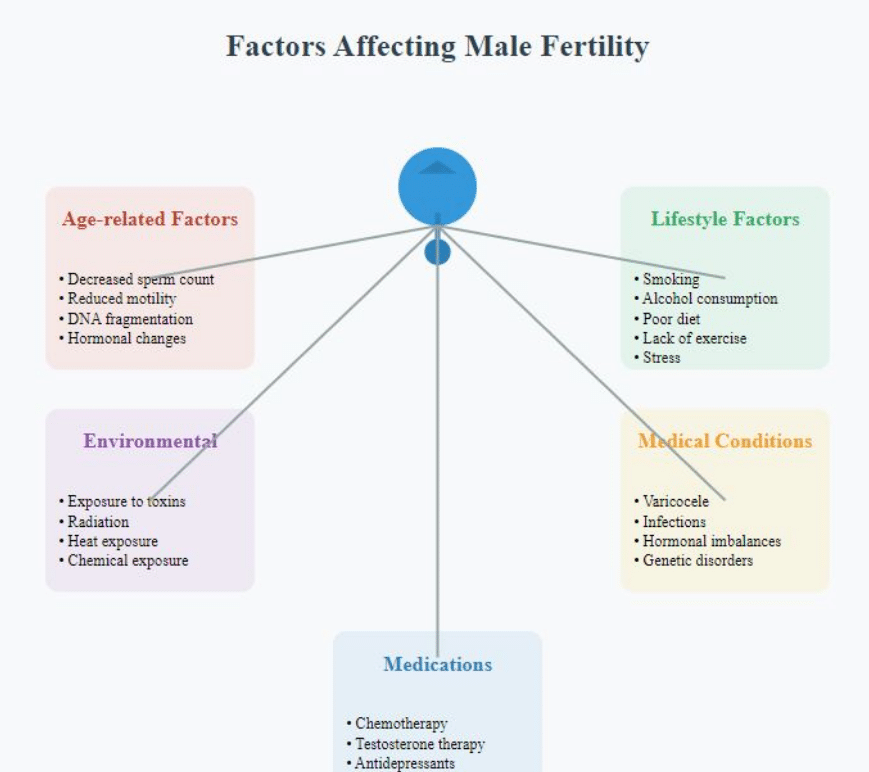
Various factors, including lifestyle habits, environmental conditions, and medical issues can influence male fertility. Being aware of these factors is important for both preventing fertility problems and seeking appropriate treatment when necessary.
Age-related factors
Although men are capable of producing sperm throughout their lives, fertility tends to decline with age. Studies have shown that male fertility typically decreases around age 35, with more pronounced changes occurring after 40.
Older men may experience a reduction in both the quality and quantity of sperm, which can affect fertility potential. Additionally, as men age, the likelihood of sperm containing DNA damage increases. This can lead to a higher risk of genetic disorders being passed on to offspring.
Lifestyle factors
Diet and nutrition play a significant role in male fertility. A well-balanced diet that is rich in antioxidants, vitamins, and minerals supports healthy sperm production. On the other hand, being overweight or malnourished can have a negative impact on sperm production.
Exercise is another key factor, as moderate physical activity can improve fertility. However, excessive or intense exercise might temporarily reduce sperm count.
Unhealthy habits like smoking can lower sperm count and affect sperm movement, while excessive alcohol consumption may lead to reduced testosterone levels and impair sperm quality.
Moreover, chronic stress can disrupt hormone levels, which in turn affects sperm production. Practicing stress management techniques can help improve fertility.
Environmental factors
Exposure to environmental toxins and chemicals, such as pesticides, heavy metals, and industrial pollutants, can harm sperm production. Men working in jobs where they are exposed to these substances should take precautions to minimize contact.
Heat exposure is another environmental factor that can negatively impact fertility. Prolonged exposure to high temperatures, such as from frequent use of hot tubs or keeping laptops on laps, can interfere with sperm production, as testicles function optimally at temperatures slightly lower than the body.
Additionally, radiation exposure, whether ionizing or non-ionizing, can damage sperm DNA, so protective measures should be taken, especially in high-risk occupations.
Medical conditions
Several medical conditions can directly affect male fertility. Varicocele, which is the enlargement of veins in the scrotum, is a common and treatable cause of male infertility as it can impair sperm quality.
Infections, particularly sexually transmitted or reproductive tract infections, can also impact fertility by causing blockages or scarring. Hormonal imbalances, resulting from disorders of the hypothalamus, pituitary gland, or testicles, can disrupt hormone production, which may reduce sperm production or function.
Certain genetic disorders, like Klinefelter syndrome or Y chromosome microdeletions, can also contribute to infertility by affecting sperm production.
Medications and treatments affecting fertility
Some medications and medical treatments can temporarily or permanently affect fertility:- Chemotherapy and radiation therapy for cancer
– Long-term use of anabolic steroids
– Some antibiotics and antidepressants
– Blood pressure medications and testosterone replacement therapy
Understanding these factors can help in identifying potential c
Diagnosing Male Infertility

Accurate diagnosis is crucial for effective treatment of male infertility. The diagnostic process typically involves several steps and may include various tests and examinations.
A. Initial consultation and medical history
Identifying the root cause of male infertility requires a comprehensive diagnostic approach that begins with a thorough consultation.
During this initial meeting, doctors gather essential information about conception attempts, overall health status, and relevant medical history including past illnesses or surgeries that might affect fertility. They also discuss sexual habits and any related concerns.
B. Physical examination
The physical examination follows, where doctors check for visible signs that might indicate fertility problems. This includes looking for hormonal imbalance indicators, examining the genital area for structural issues, and evaluating sexual development characteristics.
These observations provide valuable clues about potential underlying problems.
C. Semen analysis
This is the primary and most important test for male fertility. It evaluates:
- Sperm count: The number of sperm per milliliter of semen
– Normal count is generally considered to be 15 million or more sperm per milliliter
- Sperm motility: The percentage of sperm that are moving and how well they move
– At least 40% should be motile
- Sperm morphology: The size and shape of the sperm
– At least 4% should have a normal shape
Additional parameters like semen volume and pH are also assessed.
D. Hormone testing
Blood work helps assess hormone levels that influence sperm production. Tests measure testosterone, follicle-stimulating hormone (FSH), luteinizing hormone (LH), and prolactin. Unusual results may point to problems with either the testes or the brain’s hormone control centers.
E. Genetic testing
When genetic factors are suspected, specialized tests become necessary. These include analyzing chromosomal patterns, checking for missing Y chromosome segments, and screening for cystic fibrosis genes.
Imaging techniques like ultrasound and MRI complement these tests by revealing physical abnormalities in reproductive organs, such as blocked ducts or enlarged veins (varicoceles).
Additional specialized evaluations may include checking urine after ejaculation, testing for antibodies that attack sperm, and assessing sperm function. The combined results from all these diagnostic tools enable doctors to develop targeted treatment strategies for each individual’s situation.
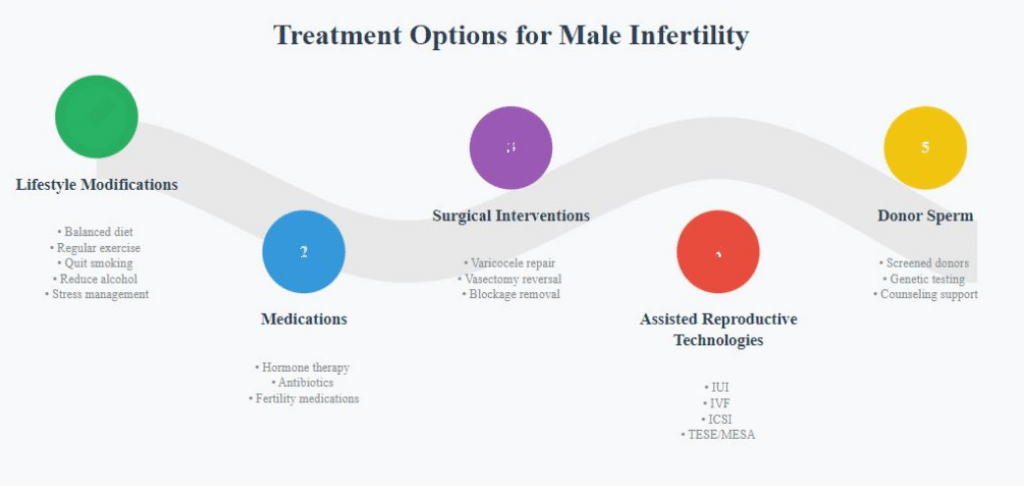
Treatment Options for Male Infertility
Treatment for male infertility depends on the underlying cause and may involve various approaches, from lifestyle changes to advanced medical procedures.
A. Lifestyle modifications
Simple lifestyle adjustments often serve as the initial step in addressing male fertility issues.
These changes include adopting a balanced diet, maintaining regular exercise routines, eliminating tobacco use, moderating alcohol intake, and minimizing exposure to harmful environmental factors. Stress management through relaxation methods can also positively impact reproductive health.
As part of lifestyle planning, couples can improve their conception chances by accurately tracking ovulation. KNOWHEN® Saliva Ovulation Test offers several unique benefits for family planning:
- Non-invasive testing using only saliva
- Reusable and cost-effective compared to disposable urine tests
- Provides up to 7 days advance notice of ovulation
- 98.9% accuracy in predicting fertile days
- Helps couples time intercourse during peak fertility windows
- Easy to use at home with results in minutes
- No need to interpret complex color changes
- Morning testing without first morning urine requirement
- Can be used alongside other fertility treatments and lifestyle changes
B. Medications and hormone therapy
When lifestyle changes prove insufficient, medical interventions become necessary. Doctors may prescribe specific medications such as human chorionic gonadotropin or clomiphene citrate to boost testosterone and sperm production.
Antibiotics treat reproductive infections, while other medicines focus on improving sperm movement or addressing erectile problems.
C. Surgical interventions
Surgical solutions target specific anatomical issues affecting fertility. Varicocele repair, which redirects blood flow by sealing problematic veins, shows improvement in 40-70% of cases.
Men who previously underwent vasectomy can opt for reversal surgery, though success rates depend on the time elapsed since the original procedure.
Additional surgical options include clearing blockages in ejaculatory ducts or correcting congenital reproductive tract issues.
D. Assisted reproductive technologies (ART)
When other treatments are unsuccessful or not applicable, ART may be recommended:
- Intrauterine insemination (IUI):
– Involves placing specially prepared sperm directly into the uterus
– Useful for mild male factor infertility or unexplained infertility
- In vitro fertilization (IVF):
– Eggs are fertilized with sperm in a laboratory setting
– Resulting embryos are then transferred to the uterus
– Can be successful even with low sperm counts
- Intracytoplasmic sperm injection (ICSI):
– A single sperm is injected directly into an egg
– Used when sperm counts are very low or sperm cannot penetrate the egg
These techniques may be combined with procedures like testicular sperm extraction (TESE) or microsurgical epididymal sperm aspiration (MESA) in cases of azoospermia (absence of sperm in ejaculate).
E. Use of donor sperm
For cases where using one’s own sperm isn’t viable, donor sperm presents an alternative path to parenthood. This option works with both intrauterine insemination and in vitro fertilization procedures. Sperm donors undergo thorough health screenings and genetic testing.
Professional counseling helps couples navigate the emotional aspects of this decision. Treatment selection ultimately depends on the specific fertility diagnosis, personal preferences, and financial resources available to each couple. A fertility specialist can help couples navigate these options and choose the most appropriate treatment plan.
Conclusion
Male fertility is a complex issue influenced by various biological, environmental, and lifestyle factors. Proper diagnosis involves a combination of physical examinations, semen analysis, and potentially more advanced tests.
Treatment options range from lifestyle modifications to advanced assisted reproductive technologies. The psychological impact of infertility on men is significant and should be addressed alongside medical treatment.
Male factor infertility contributes to a significant portion of all infertility cases. Early diagnosis and treatment can improve outcomes and reduce emotional stress. Addressing male infertility is crucial for the overall reproductive health of couples.
Men experiencing fertility issues should not hesitate to seek medical advice. A range of effective treatments and support systems are available. With ongoing research and technological advancements, the future of male fertility treatment looks promising.
Sources
https://www.auanet.org/guidelines/guidelines/male-infertility
https://www.auanet.org/guidelines-and-quality/guidelines/male-infertility
https://www.pharmacy180.com/article/anatomy-of-the-male-reproductive-system-3707/
https://www.yalemedicine.org/conditions/male-infertility
https://www.fertstert.org/article/S0015-0282(13)00687-0/fulltext
https://pubmed.ncbi.nlm.nih.gov/23809502/
https://www.sciencedirect.com/science/article/pii/S0015028213006870